Every 15 minutes, someone in the United States has brain surgery related to hydrocephalus, more commonly known as “water on the brain.” There is no cure. IUPUI’s Bonnie Blazer-Yost and colleagues are hoping to change that by creating a treatment that could eliminate the need for invasive surgery.
People with hydrocephalus have excess cerebrospinal fluid, which is what surrounds and cushions the brain, providing vital nutrients to brain tissue and the spinal cord and helping to remove toxins from the tissue. Hydrocephalic patients may experience pain, vision changes, walking disturbances and, in severe cases, brain damage and death if it is not treated.
Hydrocephalus is so common that approximately one in every 1,000 infants will be born with it. The elderly population is often affected, with many developing normal pressure hydrocephalus, which can be misdiagnosed as dementia. It can also be a side effect of traumatic brain injury or stroke.
Currently, the only effective treatment involves brain surgery and the placement of a shunt to divert the fluid from the brain to other parts of the body. According to Blazer-Yost, a professor of biology in the IUPUI School of Science and fellow of the American Physiological Society, the two-year success rate of shunts in the pediatric population is only fifty percent.
“Shunts can build up protein that prevents the fluid from draining, or they can become infected or the valves can stop working,” Blazer-Yost said. “In the majority of the cases, patients have to go through another brain surgery to revise the shunt. We are working to identify a safe drug treatment instead.”
Blazer-Yost and her team of researchers are currently testing antagonists of TRVP4, an electrolyte channel, and seeing promising results. A drug could be used as needed and for as long as a patient requires. This would be a stark difference to the uphill battle children face with shunts.
“I distinctly remember attending a meeting of the Hydrocephalus Association and sitting at a table with patients, caregivers and healthcare professionals, and each patient at my table was asked how many brain surgeries they had,” Blazer-Yost said. “Some answered as high as twenty -- by the time they were teenagers. A drug option would make a huge impact on their treatment of the disease.”
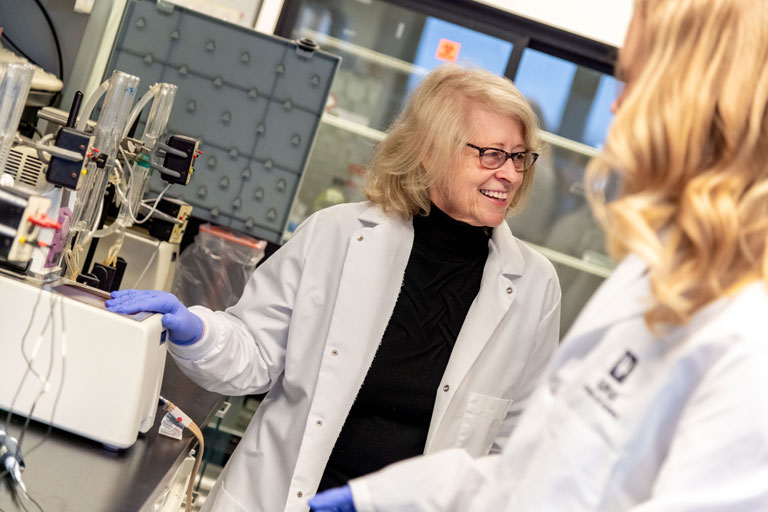
Student researchers play an integral role in Blazer-Yost’s laboratory. They are working to understand how the excess cerebrospinal fluid impacts the rest of the brain.
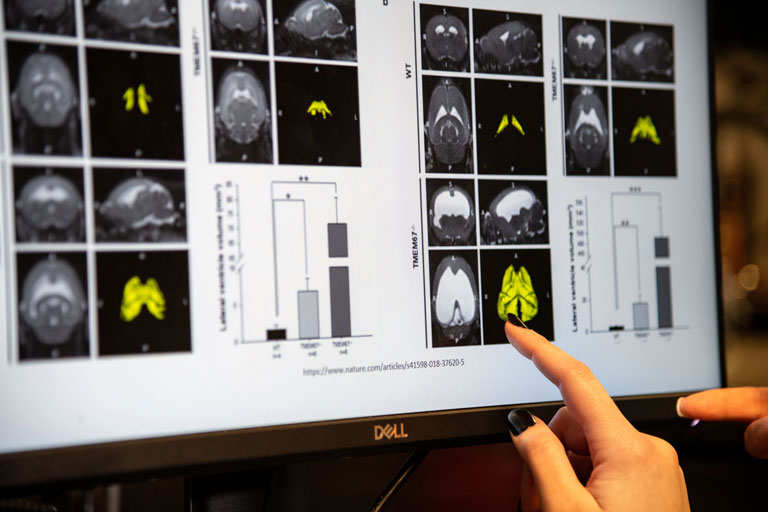
“Fluid build-up will affect the entire brain, which will in return affect overall mental function,” said Makenna Reed, a Ph.D. student working to identify what brain regions are secondarily affected by hydrocephalus. “The goal of our laboratory team is to understand the cause and effect of hydrocephalus.”
Blazer-Yost spent most of her career studying kidneys. While working to identify a drug that would target polycystic kidney disease, her team discovered a treatment that did not help kidney disease as hoped, but instead, seemed to alter the hydrocephalus in their animal models – leading her down a whole new research path.
Following this discovery, she received funding from the Indiana Clinical and Translational Sciences Institute, IU and the Hydrocephalus Association to further her research. Using the resulting preliminary data, the team received a $1.8 million grant from the Department of Defense in 2017 to study hydrocephalus and develop potential treatments.
Blazer-Yost is working with Teri Belecky-Adams, director of the Neuroscience Undergraduate Program in the School of Science, who is examining how hydrocephalus can affect vision and the optic nerve. They recently teamed up with two investigators from Johns Hopkins University, Lauren Jantzie and Dr. Shenandoah Robinson, who have unique treatments and animal models. Working together, the four researchers have expanded the research studies now aimed toward treatment for all aspects of hydrocephalus, and they are in the process of submitting joint grants to fund their ongoing collaborative studies.
“We have shown that our treatment is working to decrease the excess cerebrospinal fluid in our animal models, now we want to look at whether it reverses the effects happening in other areas of the brain like vision and also to determine if the treatments are effective in a range of other animal models,” Blazer-Yost said. “Collaborations with other researchers enhance the range of studies that are possible. These partnerships may provide synergistic interactions to enhance research that explores treatment for various forms of hydrocephalus and the side effects.”
Blazer-Yost hopes to develop a potential treatment that a company would pick up for drug development, as clinical trials would move much faster with a partner.
“We’ve been lucky so far and haven’t seen any adverse side effects in the cells or animal models,” Blazer-Yost said. “But it’s a very long process from animals to humans during the development of a drug.”
In 2019, Blazer-Yost was issued a patent for the TRPV4 hydrocephalus therapeutic, which she received with the help of the IU Innovation and Commercialization Office.